I’ve spent my entire adult life working in healthcare. As a pharmacist, I’ve counselled countless patients, navigated prescribing complexities, and witnessed the intricate dance of our NHS from the inside. For the most part, I’ve been fortunate—blessed with good health, save for the occasional chest infection, a bout of COVID, and that peculiar post-COVID gift of lower leg oedema that seemed to appear from nowhere.
This professional experience has given me what I thought was an advantage: the clinical judgment to know when something can run its natural course and when it’s time to seek that crucial second opinion. How naive I was to think that knowledge alone could shield me from becoming just another frustrated voice in an overwhelmed system.
When Professional Instinct Meets Patient Reality
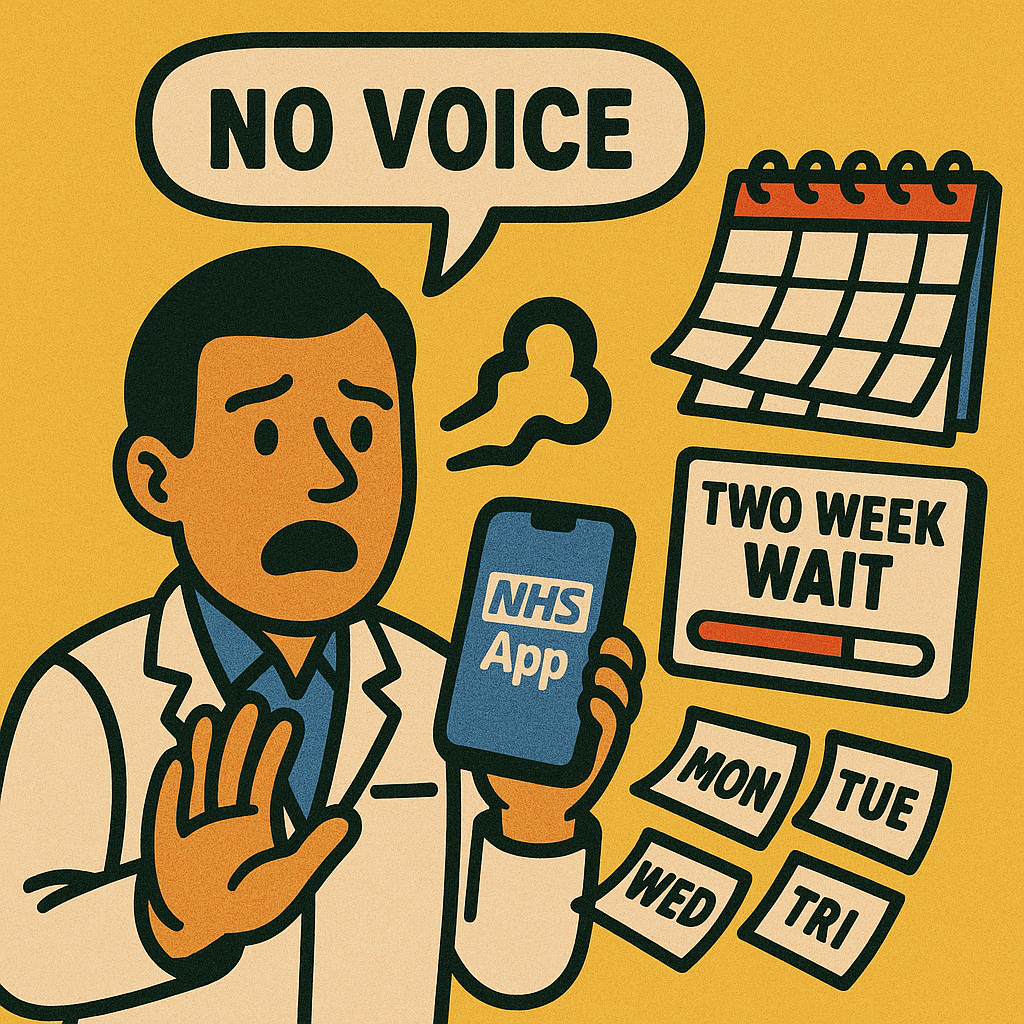
It started subtly—my voice growing huskier than usual, occasionally disappearing entirely. “Viral,” I diagnosed myself with the confidence that comes from years of clinical experience. After all, I had no other symptoms. Rest, fluids, and time—the trinity of self-care I’ve recommended to patients countless times.
But time became my enemy. Four and a half weeks passed without improvement, and now headaches and neck pain had joined the symphony of symptoms. My professional instincts were screaming for that second opinion, but accessing it? That’s where my patient journey truly began.
The Digital Queue: Modern Healthcare’s New Waiting Room
Working full-time whilst trying to navigate GP appointments is like playing a game where the rules change daily. The traditional routes—the 8 AM phone roulette or joining the very British queue snaking from surgery doors—weren’t viable options for someone with my schedule.
Fortunately, I’m what you might call a health tech enthusiast. I’m registered with both the NHS App and Airmid, my surgery’s clinical system app. Technology was supposed to be the great equaliser, bringing the NHS into the digital age and solving the access crisis. How wonderfully optimistic that seems now.
Against all odds, I managed to secure an appointment—a week away, but progress nonetheless. I dutifully added my symptom details and waited, feeling cautiously optimistic about the digital efficiency of modern healthcare.
A Glimpse of What Healthcare Could Be
Credit where it’s due: the surgery team impressed me. They reviewed my symptoms and deemed it necessary to bring me in sooner for a face-to-face appointment. For a moment, the system worked as it should—proactive, responsive, patient-centered.
The GP I saw was everything you’d want in a healthcare provider: thorough, friendly, with an excellent bedside manner. He explained that my symptoms and age placed me in a category requiring cancer exclusion via urgent referral—something I’d expected and wasn’t alarmed by. The two-week wait pathway seemed straightforward, blood sample was scheduled for the next day, and I was told to follow up if I hadn’t heard anything within two weeks.
Walking out of that appointment, I felt the NHS had functioned exactly as designed. How quickly that confidence would crumble.
When the System Breaks Down
The NHS App showed my referral as pending—a small digital comfort that made me feel connected to the process. It even helpfully prompted me to follow up if I hadn’t heard by the 23rd. Technology working for the patient—what a concept.
The 23rd arrived with silence from the hospital. I decided to give it until the end of the day before following up, clinging to the benefit of the doubt. The contact details led to an O2 messaging service where I left my information, hoping someone would return my call.
Then came the digital betrayal: all traces of my pending referral vanished from the NHS App. Gone. As if my medical need had never existed. Thankfully, my years in healthcare had taught me to keep detailed records—I had the booking reference and contact number, for whatever they were worth.
The Professional’s Paranoia
As someone who works in healthcare, I know the stories. GP colleagues have shared tales of referrals bounced back for minor clerical errors, forcing the entire process to restart. But surely not for a two-week wait cancer pathway? Surely the urgency of that designation would provide some protection against administrative failures?
My optimistic side hoped the referral was progressing silently through the NHS machinery. My professional pessimism, however, suspected that somewhere in the digital handoff between primary and secondary care, a box hadn’t been ticked or a field hadn’t been completed correctly.
The Cruel Comedy of Bureaucracy
Two days after the date I was supposed to hear back, a letter arrived informing me about my referral. The irony wasn’t lost on me—correspondence about a communication failure, arriving after its own deadline. The letter included a URL for online booking using my reference and passcode.
The punchline? The booking reference wasn’t valid. Cancelled. Rejected. Lost in the digital ether that was supposed to make healthcare more efficient.
Back to Square One
So here I am, messaging the surgery through the NHS App (with its charming two-day turnaround) and booking another appointment for next week. The wheel spins again, and I rejoin the queue of patients seeking care in our beloved but overwhelmed NHS.
The irony isn’t lost on me—as a healthcare professional, I’m part of a system I now find myself fighting against. I understand the pressures, the funding constraints, the impossible balancing act of trying to provide quality care with ever-diminishing resources. But understanding doesn’t diminish the frustration of being failed by the very system I’ve dedicated my career to supporting.
The Lost Voice Speaks
In the meantime, this patient’s voice remains unheard—both figuratively and literally. My professional knowledge hasn’t granted me special access or smoother pathways. If anything, it’s made the failures more glaring, the inefficiencies more painful to witness.
This isn’t just about my husky voice or potential diagnosis. It’s about every patient navigating these same broken processes without the benefit of healthcare knowledge or professional connections. It’s about the erosion of trust that occurs each time our NHS fails to deliver on its founding promises of care free at the point of need.
As healthcare professionals, we often talk about patient-centred care, but what happens when we become the patients? We discover that good intentions and digital solutions aren’t enough if the fundamental processes remain fractured, starved of proper funding and support.
I’ll continue fighting for my voice—both as a patient seeking care and as a professional advocating for an NHS that actually works for those it’s meant to serve.
*Updates to follow as this journey continues...*

Leave a Reply