
Innovation vs. Inertia in NHS Technology
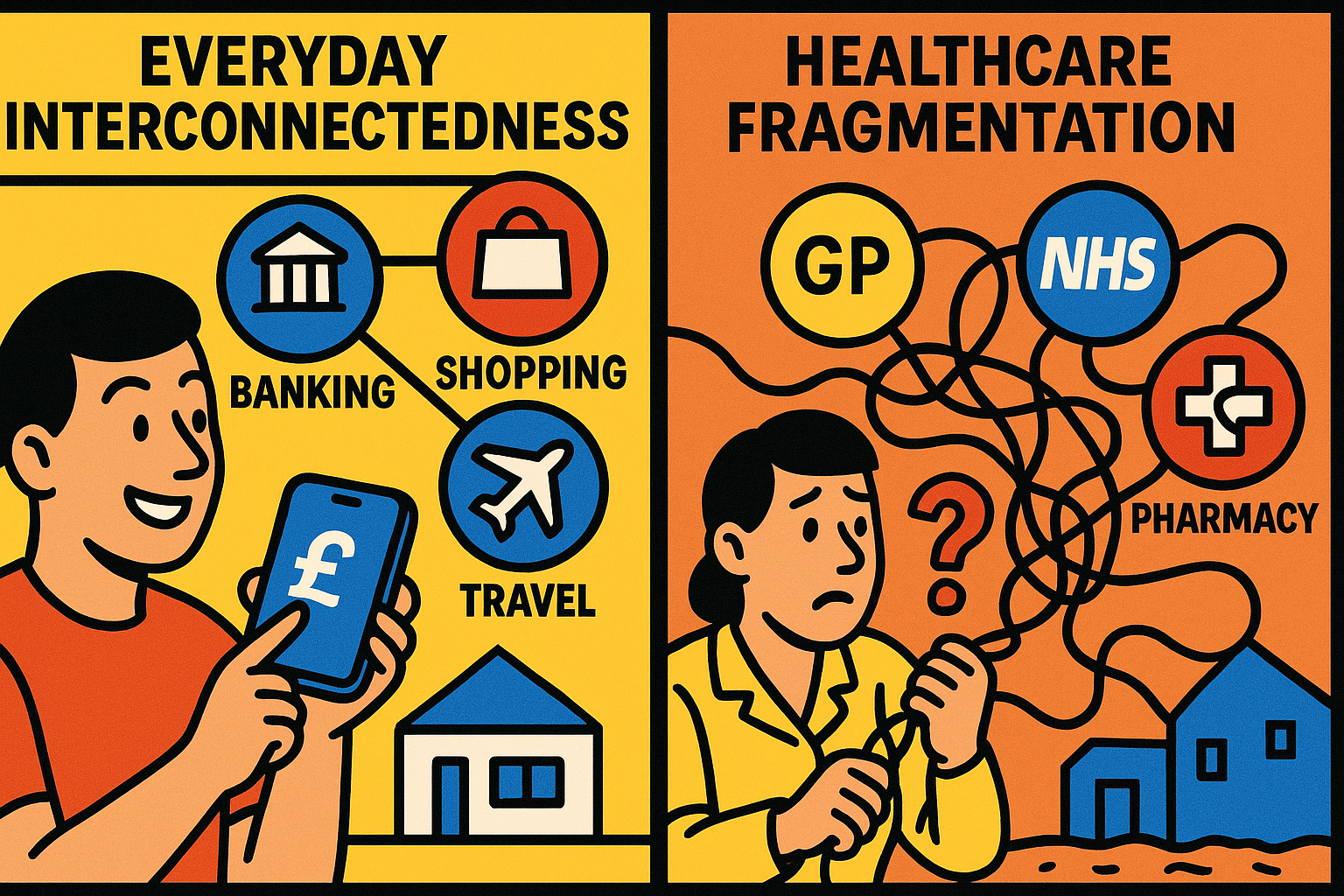
Have you noticed how our everyday lives have been transformed by seamlessly connected digital services? Banking, shopping, travel—all accessible through sleek apps that talk to each other effortlessly. Yet when it comes to healthcare technology, particularly within our NHS, things aren’t quite so fluid. Why is that?
The Green Shoots of Interoperability
There’s promising movement afoot. The NHS has begun embracing the power of interoperability—the ability for different systems to exchange and make use of information—through carefully designed APIs (Application Programming Interfaces, for the non-tech readers among us).

Take the National Patient Prescription Tracking Service as a brilliant example. This system collects data from various dispensing systems across the country into a central data store. An API then allows applications—currently just the NHS App—to present this information to patients in meaningful ways. Imagine checking the status of your prescription without phoning the GP or pharmacy. That’s the power of connected systems.
These developments aren’t just technical achievements; they represent a philosophical shift towards seeing health data as something that should flow securely where it’s needed, rather than remaining trapped in isolated systems.
The Monolith in the Room

But here’s where it gets tricky. While primary care and national services are making these strides, secondary care—our hospitals and specialist services—often operate on monolithic systems. These are the technological equivalents of massive ocean liners: powerful but slow to change direction.
Some systems weren’t built with modern interoperability in mind. They were designed to be comprehensive, all-encompassing solutions that handle everything from appointment booking to complex clinical records. Their vendors have invested millions in developing these capabilities, and they’re understandably protective of their approach.
“We’ve built everything you need,” they might say. “Why complicate things with external connections?”
It’s not an unreasonable position from their perspective. These systems work. They’re stable. They’re secure. But they may also be dampening the momentum towards a more connected healthcare ecosystem.
The Tension at Play
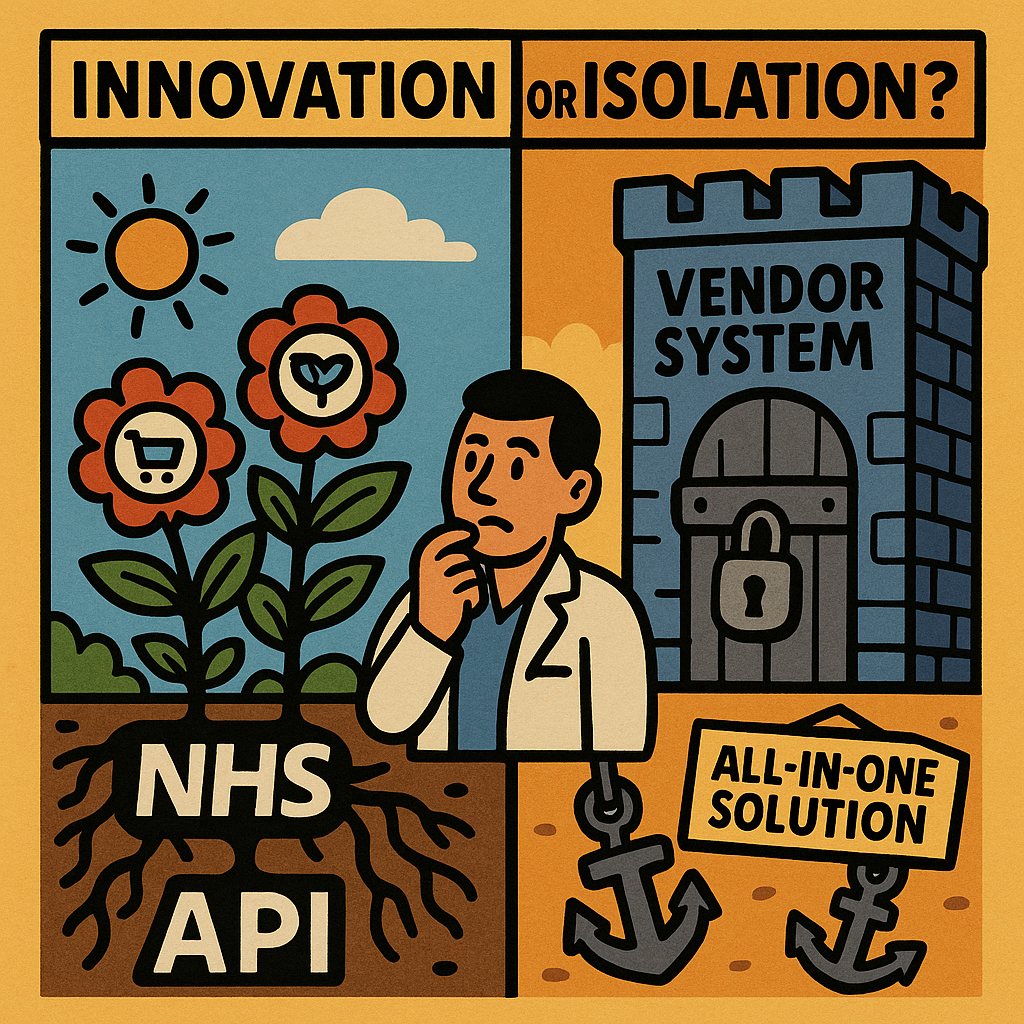
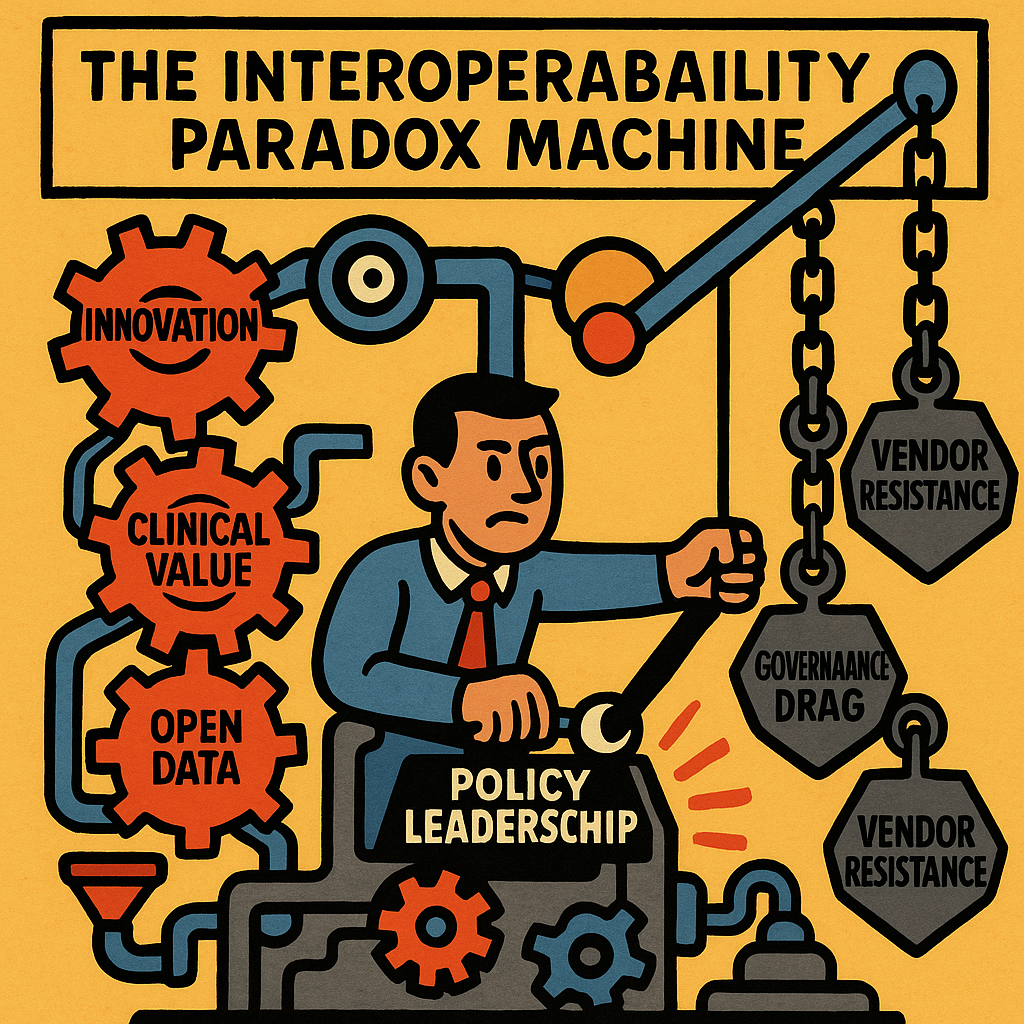
This creates a fascinating tension. On one side, we have the drive for innovation through interoperability—allowing specialist applications to flourish by accessing core NHS data through standardised APIs. On the other, we have the stability and comprehensive nature of established systems that prefer to expand their own capabilities rather than open up.
Both approaches have merits. The interoperability camp argues that no single vendor can build the best solution for every healthcare need. By creating secure ways for systems to communicate, we unleash innovation from specialists who deeply understand specific clinical or operational challenges.
The monolithic system supporters counter that healthcare is too complex and too critical for a patchwork approach. Integrated systems ensure consistency and reliability—essential qualities when lives are at stake.
What’s the Way Forward?
This is where you come in. As someone invested in the future of healthcare technology, which approach do you believe will better serve patients and clinicians?

Perhaps the answer isn’t either/or but something more nuanced. Could we maintain the stability of core systems while mandating standardised APIs that allow for innovation at the edges? Or is there value in preserving different approaches in different settings?
The stakes are high. In a resource-constrained NHS, we need technology that delivers maximum value. We need systems that support rather than hinder clinical workflows. Most importantly, we need approaches that ultimately improve patient care.
As the NHS continues its digital transformation journey, these tensions will need resolution. The question is whether we’ll actively shape that resolution through thoughtful debate and clear principles, or whether it will happen haphazardly through competing commercial interests.
What do you think? Is the future of NHS technology in robust, standardised APIs that foster an ecosystem of innovation? Or in comprehensive systems that offer end-to-end solutions? The conversation matters—and your perspective counts.
This article was created with the support of LLMs. Image creation and format and layout was created through the use of AI challenges and feedback.

Leave a Reply